Detect & Refer
Diagnostic algorithm of patients with unexplained exertional dyspnoea and/or suspected PAH1
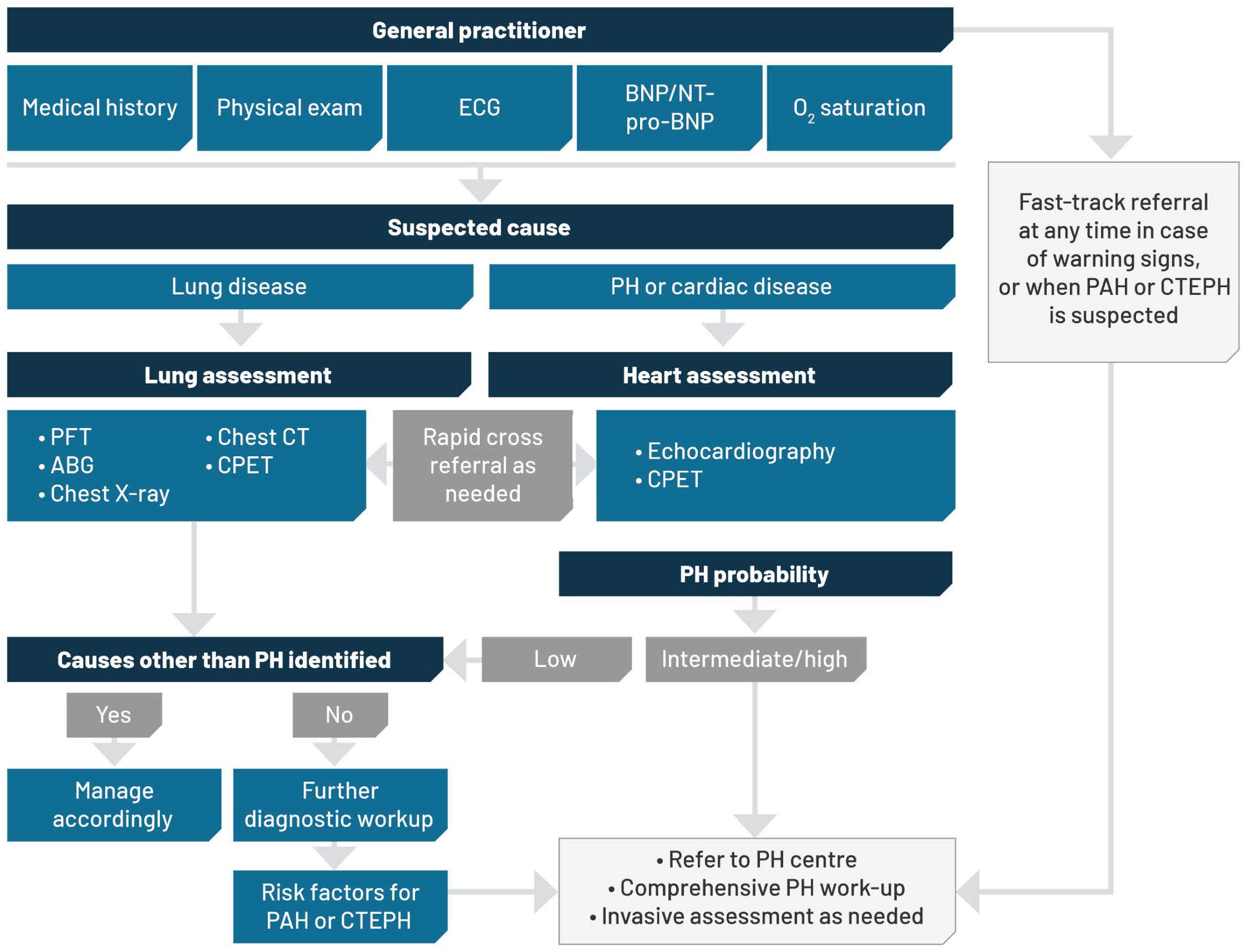
Adapted from Humbert M et al. 2022.1
This diagnostic algorithm is intended to support the referral process for suspected PAH patients. This information should not replace your specialist clinical judgement and cannot exclude the possibility of a patient having PH or PAH.
Janssen-Cilag Pty Ltd takes no responsibility for any clinical deterioration, misdiagnosis, injury or death that may arise as a result of use of information provided on this website.
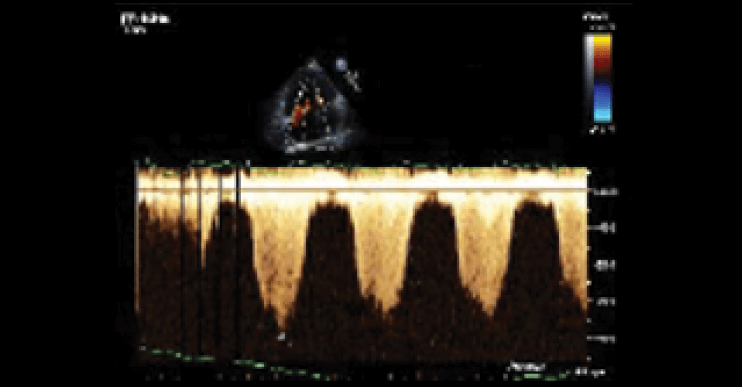
An echocardiogram that assesses the right heart as well as the left can reveal the hidden signs of PH. Always provide patient history when requesting a comprehensive echocardiogram of the heart.3,4,6
Echocardiography has become the first-line diagnostic and screening tool for PH.3,4,6 A comprehensive echocardiogram that looks at the right heart as well as the left should always be performed as part of a patient’s work-up, as it can provide evidence raising the suspicion of PH and build a case for definitive diagnosis at a PH expert centre that performs right heart catheterisation.3
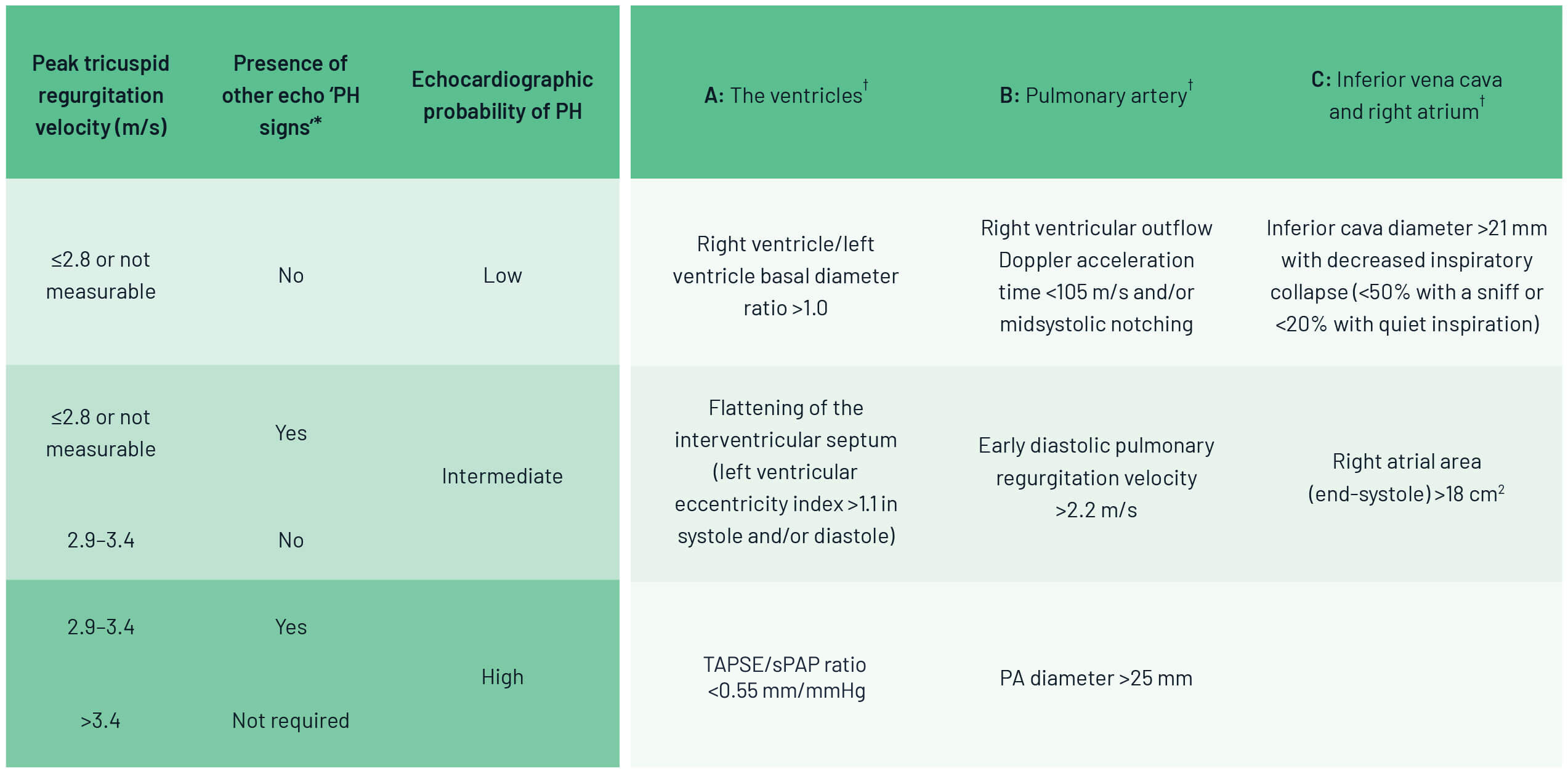
By measuring multiple echocardiographic parameters, it’s possible to determine the echocardiographic probability of PH.
Parameters include:3
- Peak tricuspid regurgitations velocity >2.8 m/s
- RV/LV basal diameter ratio >1.0
- Flattening of the IVS
- TAPSE/sPAP ratio <0.55 mm/mmHg
- RV outflow Doppler acceleration time <105 m/s and/or mid-systolic notching
- Early diastolic pulmonary regurgitation velocity >2.2 m/s
- Pulmonary artery diameter >25 mm
- IVC diameter >21 mm with decreased inspiratory collapse (sniff test)
- End-systolic RA area >18 cm2
Echocardiography (ECHO) should always be performed when PH is suspected and may be used to infer a diagnosis.3
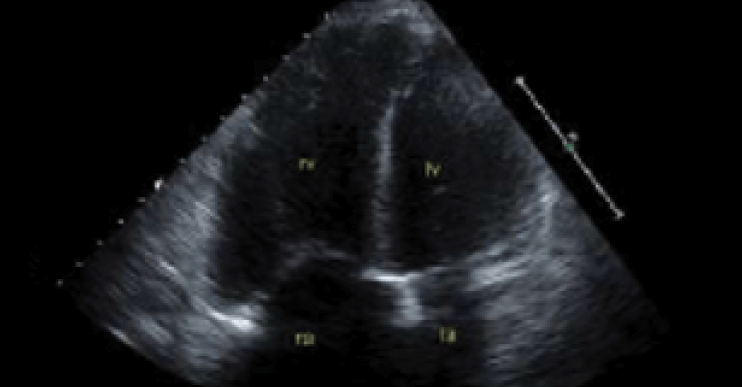
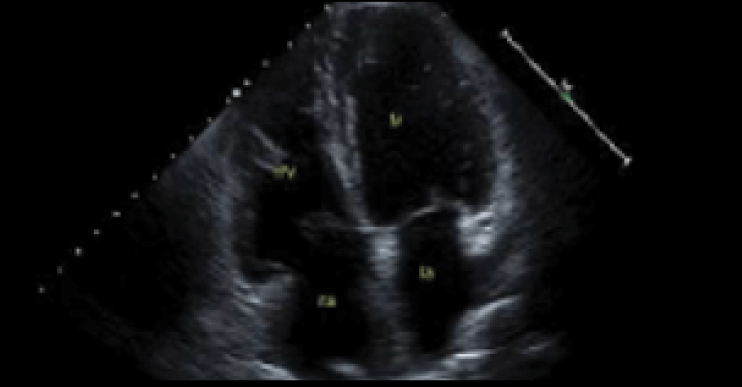
PH with evidence of cardiomegaly and enlarged pulmonary arteries
Echocardiographic probability of PH in symptomatic patients with a suspicion of PH
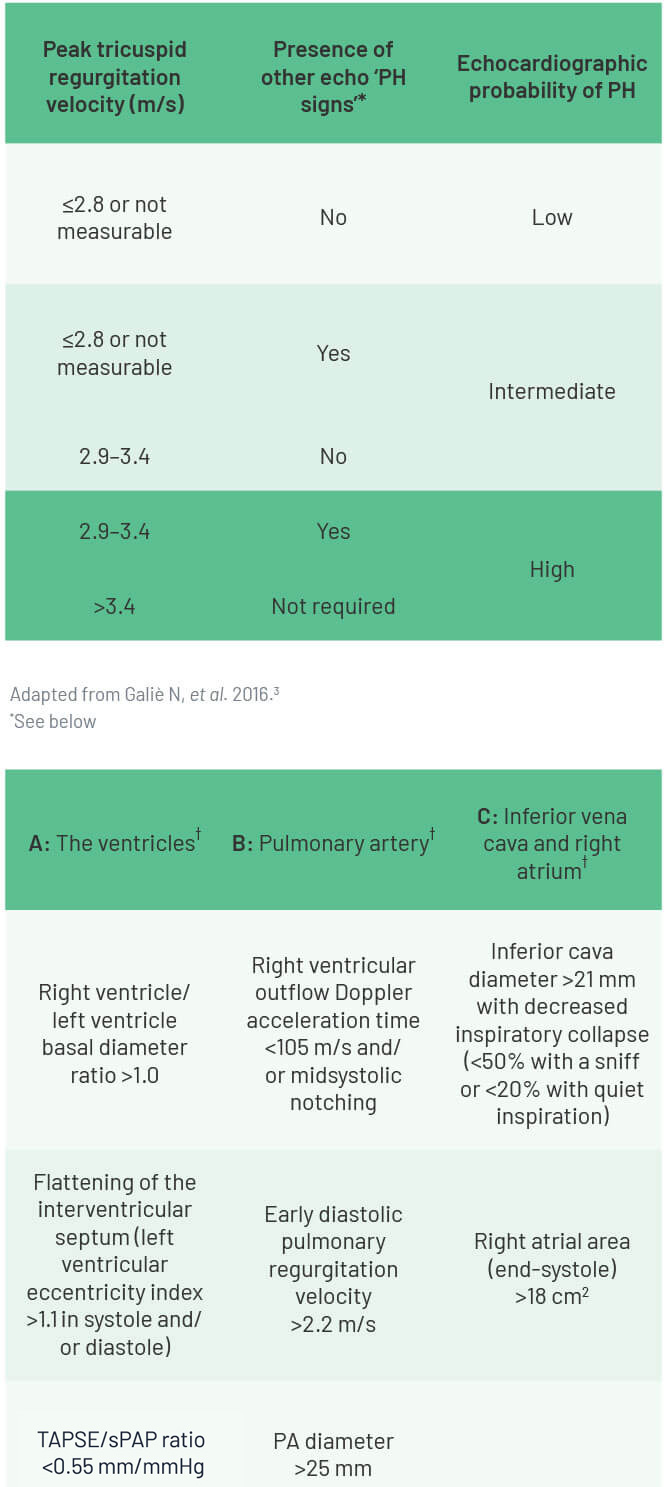
It is important to note that estimates of RA pressure may be innacurate, and therefore peak TRV is recommended (and not the estimated sPAP) as the key variable for assigning the echocardiographic probability of PH. A peak TRV >2.8 m/s may suggest PH; however, the presence or absence of PH cannot be reliably determined by TRV alone.3
Next steps when echocardiogram raises a high or intermediate probability of PH
PH is seen in many clinical conditions and is classifed into groups based on its cause.3 Treatment strategy differs between groups, so it is important to consider what might be causing PH in a patient.
PH is a common complication of underlying left heart disease and chronic lung disease.7,8 Before referring a patient with high or intermediate probability of PH for assessment at a PH expert centre, consider conducting tests to check for left heart disease or chronic lung disease.3,4 If identified, treatment of the underlying disease is the recommended approach to manage PH complications.4,7 If left heart or lung disease is not present, or if suitable tests cannot be performed, refer the patient to a PH expert centre for diagnosis.3
Other key investigations
There are several other key investigations you can perform to raise suspicion of PH and help identify and classify its cause. Note that right heart catheterisation (RHC) is required to confirm a diagnosis of PAH, and should be performed by a PH expert centre.3
Chest x-ray3
![]()
- Prominent pulmonary arteries contrasting with loss of peripheral blood vessels may be evident in PAH patients
- Right atrial and RV hypertrophy may be visible
- Signs suggestive of lung disease or left heart disease may be visible
- A normal radiograph does not exclude PH, but most patients with iPAH have an abnormal chest radiograph at the time of diagnosis
- Consider using a lateral image as well
PH with evidence of cardiomegaly and enlarged pulmonary arteries
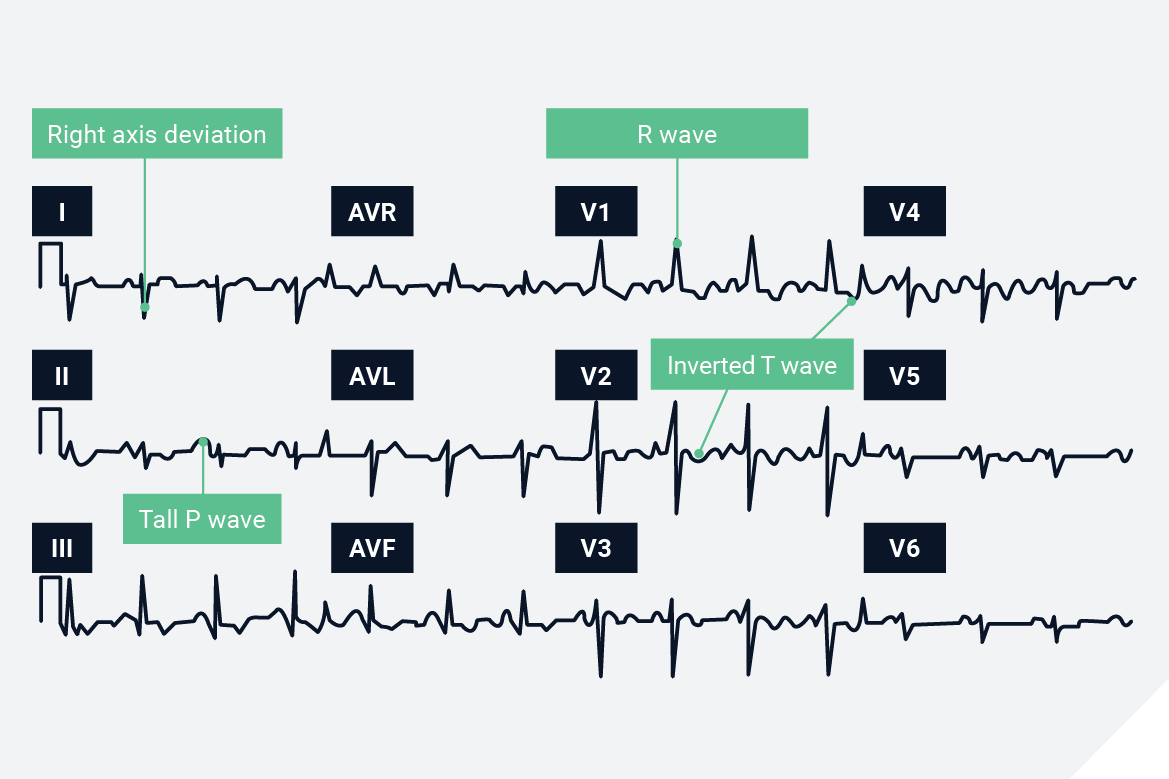
Electrocardiography (ECG)3
![]()
ECG abnormalities may not be detected in all patients with PH, and a normal ECG does not exclude the presence of severe PH.
ECG abnormalities may include:
- P pulmonale
- Right or sagittal axis deviation
- RV hypertrophy
- RV strain
- Right bundle branch block
- QTc prolongation
- Changes are indicative of RV hypertrophy only, and are not diagnostic of PH in themselves
Electrocardiographic signs of PH3
Pulmonary function testing3,9
![]()
- Although diffusion capacity can be normal in PH, most patients have decreased diffusing capacity of the lung for carbon monoxide (DLCO)
- Normal spirometry and lung volumes (or mild restriction) with reduced DLCO (40–80% predicted) is indicative of PAH
- Decreased lung volume together with a decrease in DLCO may indicate interstitial lung disease
- CT scans should be used to assess severity of emphysema or interstitial lung disease
- COPD as a cause of hypoxic PH can be diagnosed on evidence of irreversible airflow obstruction, together with increased residual volumes and reduced DLCO or increased CO2 tension
Right ventricular systolic pressure (RVSP)
![]()
RVSP is a derived parameter that is considered equal to systolic pulmonary artery pressure in most patients (in absence of pulmonary outflow obstruction). The estimation is made taking into account RAP using the simplified Bernoulli equation:3,10
RVSP=4V2 + RAP
V=velocity of tricuspid jet (TRV, metres/sec);
RAP=right atrial pressure
The value for RAP used in this equation is estimated by echocardiography based on the diameter and respiratory variation in diameter of the IVC.3 An IVC diameter <2.1 cm that collapses >50% with a sniff suggests a normal RA pressure of 3 mmHg (range 0–5 mmHg), whereas an IVC diameter >2.1 cm that collapses <50% with a sniff or <20% on quiet inspiration suggests a high RA pressure of 15 mmHg (range 10–20 mmHg).3
- RVSP >40 mmHg generally warrants further evaluation in patients with unexplained dyspnoea, in the absence of other potential aetiologies of PH, such as left heart disease or advanced lung disease 10
- In PH, a study utilising data from the National Echo Database Australia (NEDA) found that patients with eRVSP >30 mmHg have a significantly increased risk of mortality11
Right heart catheterisation (RHC)
![]()
RHC is required to definitively diagnose PAH and CTEPH, as it is the only way to directly and accurately measure haemodynamic impairment and to undertake vasoreactivity testing.3 RHC should only be performed once other investigations have been completed with the objective of answering specific diagnostic questions, particularly pertaining to haemodynamics in the context of echocardiographic findings. 3
Due to its technically demanding nature and the meticulous attention to detail required to obtain clinically useful information, RHC should only be performed in PH expert centres.3 As well as helping to provide the most useful clinical information, this will help to ensure patients are not put at unnecessary risk.3
RHC should only be performed at PH expert centres, where the risk of morbidity and mortality are low (1.1% and 0.055%, respectively).3 If, based on your investigations, you suspect PAH, the best practice is to refer your patient to a PH expert centre as soon as possible.3
Footnotes
ABG: arterial blood gas; BNP: brain natriuretic peptide; CBC: complete blood count; CHD: congenital heart disease; COPD: chronic obstructive pulmonary disease; CPET: cardio-pulmonary exercise test; CT: computed tomography; CTD: connective tissue disease; CTEPH: chronic thromboembolic pulmonary hypertension; DLCO: diffusing capacity of the lung for carbon monoxide; ECG: electrocardiography; HIV: human immunodeficiency virus; HR-CT: high-resolution CT; iPAH: idiopathic PAH; IVC: inferior vena cava; mPAP: mean pulmonary arterial pressure; NT-proBNP: N-terminal pro-brain natriuretic peptide; PA: pulmonary angiography; PAH: pulmonary arterial hypertension; PAW: pulmonary artery wedge pressure; PFT: pulmonary function tests; PH: pulmonary hypertension; PVOD/PCH: pulmonary veno-occlusive disease or pulmonary capillary hemangiomathosis; PVR: pulmonary vascular resistance; RA: right atrium; RHC: right heart catheterisation; RV: right ventricle; RVSP: right ventricular systolic pressure; TRV: tricuspid regurgitation velocity; V/Q: ventilation/perfusion.
References
- Khou V et al. Respirology 2020;25(8):863–71.
- Strange G et al. Pulm Circ. 2013;3:89–94.
- Humbert M et al. Eur Heart J 2022;43(38):3618–3731.
- Frost A et al. Eur J Resp J 2019;53:1801904.
- Simonneau G et al. Eur Respir J 2019;53:1801913.
- Vachiry J-L et al. Eur Respir J 2019; 53: 1801897.
- Nathan SD et al. Eur Respir J 2019; 53: 1801914.
- Bossone E et al. J Am Soc Echocardiogr 2013;26(1):1–14.
- Galiè N et al. Eur Resp Rev J 2009;34:1219–63.
- Rudski LG et al. J Am Soc Echocardiogr 2010;23:685–713.
- Strange G et al. J Am Coll Cardiol 2019;73(21):2660–72